Message from the Chair & Chief, Pediatrics
 The Department of Pediatrics at McMaster University and McMaster Children’s Hospital is home to over 200 pediatricians, scientists, teachers, and trainees whose collective mission is to improve the well-being of children and their families – both locally, and around the world.
The Department of Pediatrics at McMaster University and McMaster Children’s Hospital is home to over 200 pediatricians, scientists, teachers, and trainees whose collective mission is to improve the well-being of children and their families – both locally, and around the world.
Our mission is underpinned by values of collaboration, innovation, compassion, and respect. This culture informs the way we engage, and the result is a supportive and vibrant academic environment where, we believe, almost anything is possible.
Our faculty contribute to 19 divisions that reflect the comprehensive spectrum of pediatric subspecialties. We provide our clinical expertise to the infants, children, and youth who visit us at McMaster Children’s Hospital and the Ron Joyce Children’s Health Centre, and through partner institutions across the Hamilton Health Sciences, St. Joseph’s Healthcare Hamilton, and Niagara Health. Collectively, we serve a population of 2.5 million people from south central Ontario and the surrounding regions.
Follow us on Social Media
To stay up to date on news, events and research, follow us on any of our platforms.
Latest News

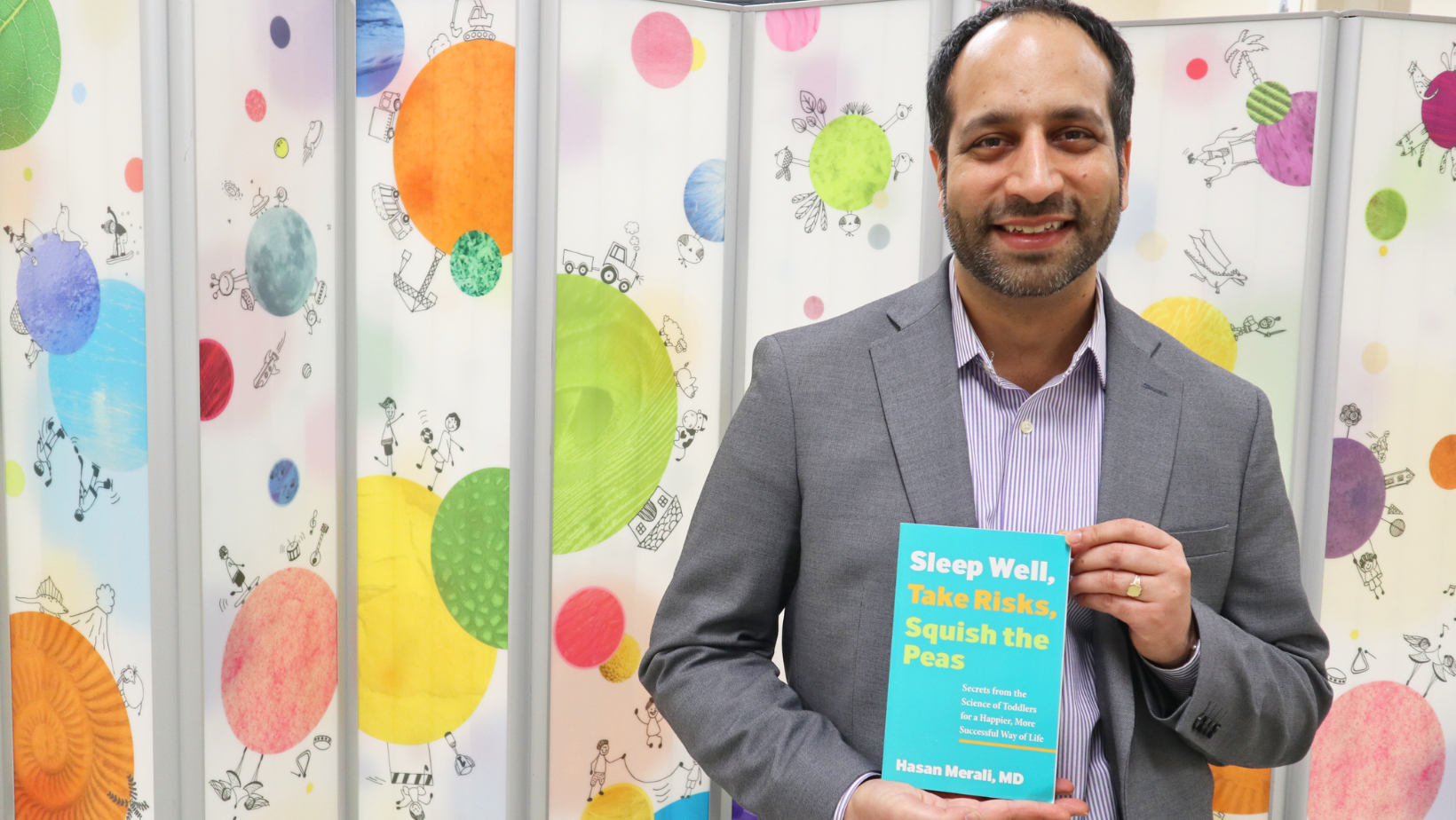
Popular Science ➚
After 100 years, new guidelines propose rules for common food allergy treatment
Pediatrics in the Media
Faculty of Health Sciences ➚
McMaster researchers create first-ever guidelines to help kids build tolerance to food allergens
FHS

Brighter World ➚
McMaster Child Health Research Day charts the future of pediatric health
Research in the Media

Faculty of Health Sciences ➚
Charting the future of child health: McMaster University hosts collaborative research day
FHS

Faculty of Health Sciences ➚
Common activities emergency doctors say they would avoid this spring
FHS



Faculty of Health Sciences ➚
Measles: What a pediatric infectious disease expert wants you to know
News